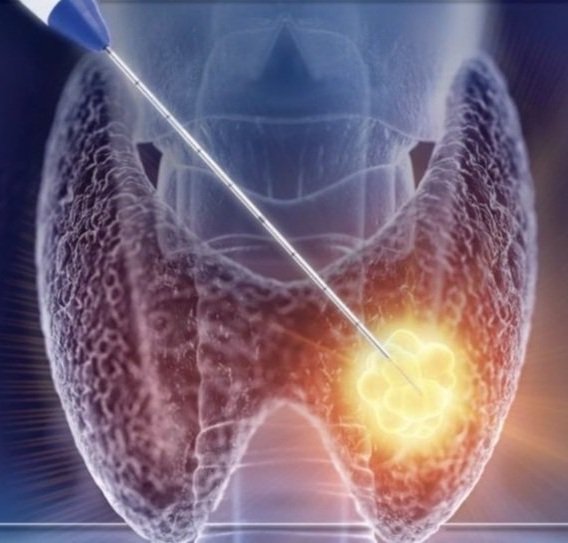
Thyroid Radiofrequency Ablation
What is RFA
Radiofrequency ablation (RFA) is a procedure that uses heat to shrink a thyroid nodule (buildup of cells). This non-surgical outpatient procedure involves an ultrasound that guides the physician as they insert a needle electrode into the thyroid. The electrode applies heat to ablate (surgically remove) the nodule. Typically, the resultant decreased size of the thyroid nodule can eliminate symptoms and improve the patient's aesthetics.
Thyroid RFA can decrease the size of thyroid nodules by at least 80%
Approved: STARmed’s radiofrequency ablation technology is the only available RFA tool created to treat thyroid nodules
Indications
RFA may be recommended to treat:
Solid or partially cystic benign (non-cancerous) thyroid nodules causing symptoms or cosmetic issues
Benign thyroid tumours (adenomas) that are functioning independently
Toxic or pretoxic cancerous micropapillary tumours
Cancer cells that have spread to the lymph node that do not improve with radioiodine
Individuals who cannot undergo surgery
Contradictions
RFA should be avoided in the following cases:
The nodule is known to be cancerous
Suspicious characteristics on sonograph imaging despite non-cancerous biopsy results
Cystic or mostly cystic thyroid nodules
Heart conditions that disrupt electrode placement
Pregnancy
Ultrasound does not allow complete visualization of entire nodule
FAQs
-
Tests:
Your doctor may request that you undergo repeat studies before the procedure (ultrasound, biopsy, bloodwork, etc.). The results must be received by our team two weeks pre-procedure.
Medications:
Stop taking medications (aspirin, coumadin, Plavix, Xarelto) or herbal supplements that can thin your blood (ginseng, turmeric fish oil, elderberry, etc.) 5 days before the procedure if your doctor says that it is safe to do so. Please inform us if it is unsafe.
-
You may take your regular medications (except those listed above) and eat/drink until the appointment.
A family member/friend should escort you home after the procedure.
Arrive 15 minutes before the appointment. You may wear undergarments/clothes that permit access to your neck, upper chest and thighs. After checking in, take 400 mg of Motrin/Advil or 440 mg Aleve or 1000 mg Tylenol, and Xanax (if prescribed).
-
A local anesthetic will numb your neck
If you have larger nodules, your surgeon may use an injection(s) to block the nerves in your neck that promote pain. This procedure can cause temporary visual blurriness, dizziness, warmth and neck heaviness.
Discomfort is expected during the procedure. You may experience pressure growing in the neck and "popping" sensations. Inform your surgeon if you experience any unusual feelings and they can reassure you if it is normal or temporarily pause the procedure to reduce the pressure.
Observation period: When the procedure finishes, you will rest and be observed for 1 hour before going home. You might feel light-headed, dizzy, or nauseous. These feelings should return to normal before you go home.
-
Neck Discomfort
Neck discomfort is expected within the first 48-72 hours after the procedure.
Pain management:
Your surgeon may prescribe you with Prednisone to take after the procedure to reduce inflammation/ swelling or Xanax to promote relaxation
If prescribed, obtain these medications before the procedure date. You may want to purchase Ibuprofen/Motrin/Advil, Aleve, or Extra Strength Tylenol.
To minimize swelling and inflammation:
Place ice compresses on your neck as much as possible within the first 24 hours following the procedure. Continue taking Motrin/Advil/Aleve/Extra Strength Tylenol with meals for the first 48 hours.
If your surgeon prescribed you with a steroid taper, take the first dose as soon as possible after the procedure. Eat food before each dose. You will take 20 mg on day 1, 10 mg on day 2, and 5 mg on day 3.
Bruising
Bruising may occur a day after the procedure, particularly in people with large nodules or nodules with many blood vessels. Bruising may be found on the neck or chest and will usually return to normal itself.
NOTIFY OUR TEAM OF THE FOLLOWING
Fever over 101.5°F/38.5°C
Significant difficulty breathing, drinking or eating
Discharge (fluid) from the puncture area(s)

